What are Varicose Veins?
Dr. Francis SANWO
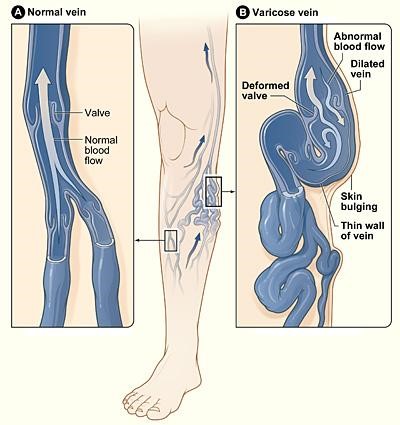
Varicose veins also known as varicoses or varicosities are enlarged, swollen, and twisting veins, often appearing blue or dark purple.
They occur when veins become enlarged, dilated, and overfilled with blood. Varicose veins typically appear swollen and raised, and have a bluish-purple or red color.
The condition is very common, especially in women. Around 25 percent of all adults have varicose veins. In most cases, varicose veins appear on the lower legs.
The veins rarely need treatment for health reasons, but if swelling, aching, and painful legs result, and if there is considerable discomfort, treatment is available.
Varicose veins occur when veins aren’t functioning properly. Veins have one-way valves that prevent blood from flowing backward. If the walls of the veins become stretched and less flexible, the valves becomes weak, they fail and blood begins to collect in the veins rather than continuing toward the heart. The veins then enlarge. Experts are not sure why the walls of veins stretch or why the valves become faulty. In many cases, it occurs for no clear reason. The veins furthest from the heart are most often affected, such as those in the legs thus varicose veins often affect the legs. This is because gravity makes it harder for blood to flow back to the heart.
Symptoms.
The primary symptoms of varicose veins are highly visible, misshapen veins, look twisted, swollen, and lumpy (bulging). The veins are blue or dark purple usually on your legs. You may also have pain although in the majority of cases, there is no pain. There may be swelling, heaviness, and achiness over or around the enlarged veins, especially after exercise or at night.
A minor injury to the affected area may result in longer bleeding than normal. There may be a shiny skin discoloration near the varicose veins, usually brownish or blue in color. Venous eczema (stasis dermatitis) – skin in the affected area is red, dry, and itchy. When suddenly standing up, some individuals experience leg cramps.
In some cases, you can develop swelling and discoloration. In severe cases, the veins can bleed significantly, and ulcers can form.
Complications.
Any condition in which proper blood flow is undermined has a risk of complications. However, in the majority of cases, varicose veins have no complications. If complications do occur, they may include: bleeding, thrombophlebitis: blood clots in the vein of the leg cause inflammation of the vein.
Chronic venous insufficiency – the skin does not exchange oxygen, nutrients, and waste products with the blood properly because the blood flow is weak. Chronic venous insufficiency is not caused by varicose veins, but the two entities are closely related.
People with chronic venous insufficiency may develop varicose eczema, lipodermatosclerosis (hard and tight skin), and venous ulcers. Venous ulcers classically form around ankles and are often preceded by a discolored area. It is important to get medical evaluation for chronic venous insufficiency.
Risk factors. Any condition that puts pressure on the abdomen has the potential to cause varicose veins; for instance, pregnancy, constipation and, in rare cases, tumors. Other potential risk factors include: menopause, being aged over 50 (due to wear and tear on vein valves), standing for long periods, family history of varicose veins and obesity. The following are also linked to a higher risk of having varicose veins: Gender: Varicose veins affect women more often than males. It may be that female hormones relax veins. If so, taking birth control pills or hormone therapy (HT) might contribute. Genetics: Varicose veins often run in families.
Pregnancy and varicose veins. Women are much more likely to develop varicose veins during their pregnancy than at any other time in their lives. Pregnant women have much more blood in their body; this places extra pressure on the circulatory system.
Additionally, changes in hormone levels can lead to a relaxation of the blood vessel walls. Both these factors raise the risk of having varicose veins.
As the uterus (womb) grows, there is more pressure on the veins in the mother’s pelvic area. In the majority of cases, the varicose veins go away after the pregnancy is over; this is not always the case, and sometimes, even if the varicose veins improve, there may be some left visible. Diagnosis
A physical examination, mainly visual, by a doctor will decide whether or not a patient has varicose veins. The patient will be asked to stand while the doctor checks for signs of swelling.
The following diagnostic tests are sometimes ordered:
Doppler test: An ultrasound scan to check the direction of blood flow in the veins. This test also checks for blood clots or obstructions in the veins.
Depending on the location, a venogram may be done to further assess your veins. During this test, your doctor injects a special dye into your legs and takes X-rays of the area. The dye appears on the X-rays, giving your doctor a better view of how your blood is flowing.
Tests such as ultrasounds or venograms help ensure that another disorder like a blood clot or a blockage isn’t causing the pain and swelling in your leg.
Treatment
If the patient has no symptoms or discomfort and is not bothered by the sight of the varicose veins, treatment might not be necessary. However, if there are symptoms, treatment may be required to reduce pain or discomfort, address complications, such as leg ulcers, skin discoloration, or swelling. Some patients may also want treatment for cosmetic reasons.
If lifestyle changes aren’t working, or if your varicose veins are causing a lot of pain or damaging your overall health, your doctor might try an invasive procedure. This may be surgical, use of chemical or radiofrequency.
Prevention. To reduce the risk of developing varicose veins, the following lifestyle changes may help prevent them from forming or becoming worse: avoid standing for extended periods of time, lose weight or maintain a healthy weight and exercise to improve your circulation. If you already have varicose veins, you should take these steps to prevent new varicose veins. You should also elevate your legs whenever you’re resting or sleeping.
Using compression socks or stockings may also help. These place enough pressure on your legs so that blood can flow more easily to your heart. They also decrease swelling. Varicose veins normally get worse over time. This is true even if you make the necessary lifestyle changes to control them and manage your pain. While they may be unsightly, they usually don’t cause any long-term medical problems.
Self-care tips for varicose veins. If you have varicose veins, try to improve circulation: Wear compression stockings. Wearing compression stockings is often the first approach to try before other treatments. Walk. Walking is a great way to get the blood circulating in your legs. Ask your doctor about an appropriate activity level for you. Elevate your legs. When sitting or lying down, elevate your legs above the level of your heart. Do this 10 to 15 minutes three or four times daily.
Don’t sit or stand for long periods. Change your position frequently. During long car trips, stop to take a brief walk every couple of hours. On flights, walk through the cabin about once every hour. Don’t sit with your legs crossed. Remember to wear your compression stockings when traveling. Watch what you wear. Panty-leg girdles can restrict circulation. Avoid high heels. Control your weight. Being overweight puts extra pressure on your veins.
Top of Form
Bottom of Form



Leave a Comment